Cantharidin Topical Solution
Cantharidin topical solution is a liquid vesicant medication comprised primarily of cantharidin and acetone. Cantharidin is a chemical derived from the secretions of one of several different types of blister beetles. When applied to the skin cantharidin causes blister formation.
Edge Pharma’s Cantharidin Topical Solution has the same active ingredient as Cantharone® and Canthacur®. Due to compounding pharmacy regulations, US-based practices cannot purchase non-patient specific office use cantharidin from Canadian-based pharmacies. Cantharidin also cannot be purchased from traditional (503A) compounding pharmacies for office use, since these facilities do not maintain the proper process controls and undergo the required testing to ensure the product is safe for office use. Cantharidin from Edge allows practices to both be in compliance, as well as be secure the product is made in an FDA registered and inspected outsourcing facility.
Qualified practitioners can buy Cantharidin Topical Solution in a 10 ml glass multi-dose bottle without providing patient names. Our online system makes purchasing cantharidin quick and easy.
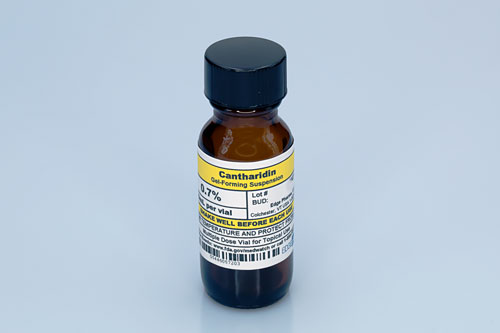
Cantharidin Gel-forming Suspension
- Cantharidin 0.7%
- Storage: room temperature
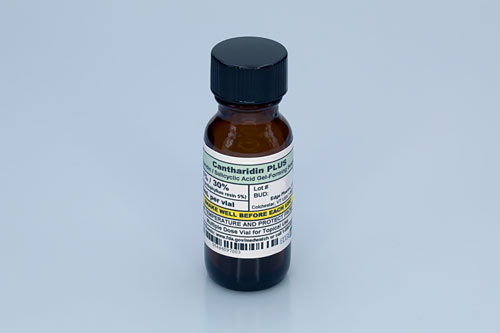
Cantharidin Plus Gel-forming Suspension
- Cantharidin 1.0%
- Salicylic Acid 30.0%
- Contains Podophyllum Resin
- Storage: room temperature
Literature Review
“Molluscum contagiosum and warts are benign epidermal eruptions resulting from viral infections of the skin.”(1) “Topical cantharidin is routinely used for the treatment of molluscum contagiosum and warts.”(2) Cantharidin is a natural toxin produced by the blistering beetle, and it has vesicant and keratolytic features.(3) According to an article in Podiatry Today: “Keratolytics are designed to peel off layers of skin. When using the medication on a wart, the wart will shrink in size in time until it is gone.” When the physician applies the keratolytic agent to the wart, the skin develops a blistering action. “The wart or part of the wart lifts off, usually within 12 hours.”(4)
A review of 20 studies, which included 1,752 patients (ages three months to 62 years) concluded that “cantharidin demonstrated clearance of warts, particularly in combination with podophyllotixin and salicylic acid, and modest benefit for pediatric molluscum contagiosum with good tolerability and safety.”(5)
A review of clinical literature on cantharidin, published in Dermatology Online Journal, identified 37 articles that included the term “cantharidin” combined with “warts,” “plantar warts,” “verucca vulgaris,” “periungal,” “subungual,” “topical treatment,” “topical therapy for warts,” “molluscum contagiosum,” “perforating collagenosis,” and “acantholysis.” “The majority of studies show that catharidin is an effective and safe treatment for removal of warts and molluscum contagiosum. Several studies also show potential novel applications of cantharidin in acquired perforating dermatosis, acute herpes zoster, and leishmaniasis.”(6)
(1) Stulberg, Daniel L., MD, Hutchinson, Anne Galbraith MD, American Family Physician, online article, Molluscum Contagiosum and Warts https://www.aafp.org
(2) Vakharia, Paras P., Chopra, Rishi, Silverberg, Nanette B., Silverberg, Jonathan, American Journal of Clinical Dermatology, online article, Efficacy and Safety of Topical Cantharidin Treatment for Molluscum Contagiosum and Warts: A Systematic Review https://link.springer.com
(3) Al-Dawsari, N.A., Masterpol, K.S., SKINmed, online article, Cantharidin in Dermatology https://www.researchgate.net
(4) Fishco, William, Podiatry Today, online article, Current Concepts in Managing Plantar Warts https://www.podiatrytoday.com
(5) Vakharia, Paras P., Chopra, Rishi, Silverberg, Nanette B., Silverberg, Jonathan, article in the American Journal of Clinical Dermatology, Efficacy and Safety of Topical Cantharidin Treatment for Molluscum Contagiosum and Warts: A Systematic Review https://link.springer.com
(6) Torbeck, Richard, Pan, Michael, DeMoll, Ellen, Levitt, Jacob, Dermatology Online Journal, Cantharidin: A Comprehensive Review of the Clinical Literature
References
1) Al-Dawsari NA, Masterpol KS. “Cantharidin in Dermatology.” PubMed.gov. https://www.ncbi.nlm.nih.gov/pubmed/27319954
“Cantharidin is natural toxin produced by the blistering beetle. It has both vesicant and keratolytic features by inducing acanthloysis through targeting the desmosomal dense plaque, leading to detachment of the desmosomes from the tonofilaments. There are two available liquid preparations for dermatologic use, Canthacur (0.7% cantharidin) and Canthacur PS (1% cantharidin 30%/salicylic acid/2% podophylotoxin). The former preparation is indicated for the treatment of common warts, periungual warts, and molluscum contagiosum, while the more potent latter preparation is indicated only for plantar warts. Both preparations provide painless applications with outcomes similar to other treatment modalities for warts and molluscum contagiosum; however, neither is approved by the Food and Drug Administration (FDA).”
2) Kartal Durmazlar, Selda Pelinxs, Damla Atacan, and Fatma Eskioglu. “Cantharidin treatment for recalcitrant facial flat warts: a preliminary study.” Journal of Dermatological Treatment 20.2 (2009): 114-119.
“All the patients were clinically cured within 16 weeks and the number of required sessions for complete clearance was 2.6 ± 1.18.”
“Cantharidin therapy was well tolerated, with mild adverse events related to skin. Conclusion: Cantharidin is safe and effective when applied to flat warts without occlusion for 4–6 hours every 3 weeks till clear.”
3) Torbeck, Richard; Pan, Michael; de Moll, Ellen; & Levitt, Jacob. “Cantharidin: A Comprehensive Review of the Clinical Literature.” Dermatology Online Journal, 20(6). doj_22861. (2014) Retrieved from: http://escholarship.org/uc/item/45r512w0
“The incidence of adverse effects associated with cantharidin for MC are: blistering (92%), erythema (37%), pain (14%), burning (10%), and pruritus (6%). Despite these adverse effects, 95% of parents polled stated they would choose cantharidin for MC treatment.”
“Cantharidin has been used to manage flat, palpebral, plantar, periungual, and subungual warts in an office setting.”
“When compared to cryotherapy, cantharidin required fewer treatments to achieve resolution (4.14 vs. 2.71). The rate of recurrence with cantharidin treatment was low, with no recurrences at six months in 144 patients with flat warts and only 1 recurrence at 1 year for digital/periungual warts.”
“Potential novel applications of cantharidin include application in acquired perforating dermatosis, acute herpes zoster, and leishmaniasis.”
4) López López, D., Vilar Fernández, J. M., Losa Iglesias, M. E., Álvarez Castro, C., Romero Morales, C., García Sánchez, M. M. and Becerro de Bengoa Vallejo, R. (2016), “Efficacy and Safety of Topical Cantharidin Treatment for Molluscum Contagiosum and Warts: A Systematic Review. 29: 269–273. doi:10.1111/dth.12356
“All patients reported treatment, supporting our results that CPS [Cantharidin-Podophylotoxin-Salicylic Acid] is a safe and efficacious treatment modality for RPW and should be considered when symptomatic infection necessitates treatment.”
5) Vakharia PP, Chopra R, Silverberg NB, Silverberg JI, Am J Clin Dermatol. 2018 Dec, “Safety and Effectiveness of Cantharidin–Podophylotoxin–Salicylic Acid in the Treatment of Recalcitrant Plantar Warts: A Systematic Review. https://www.ncbi.nlm.nih.gov/pubmed/30097988
“Topical cantharidin demonstrated clearance of warts, particularly in combination with podophyllotixin and salicylic acid, and modest benefit for pediatric molluscum contagiosum with good tolerability and safety.”
Register To Order Online
We are currently licensed to sell to all US states except Alabama and Virginia. To purchase cantharidin topical solution please fill in the registration form. Medical, DEA, or hospital pharmacy licenses will be required.
Create an account to order
Log-In if you have an account

